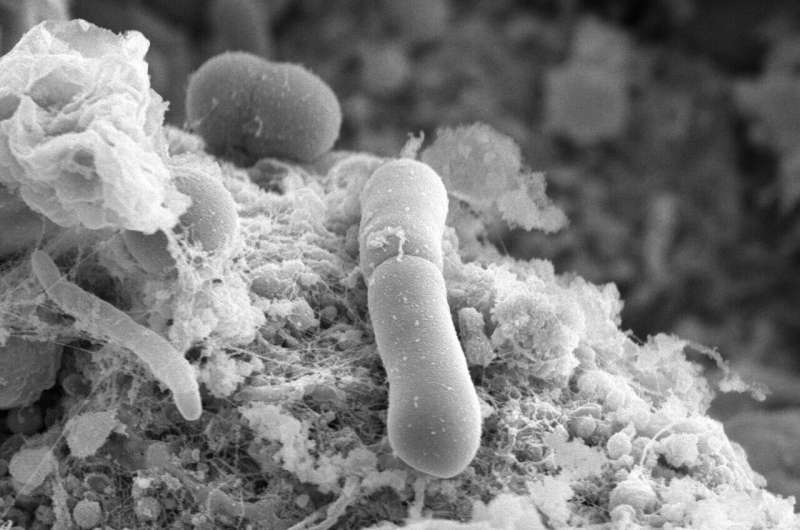
Clostridioides difficile (C. diff), a bacterium that often affects those who have recently taken antibiotics, is responsible for about 2,000 deaths annually in the UK.
A recent study conducted by researchers from the University of Sheffield and the University of Manchester reveals that C. diff can quickly develop vancomycin resistance, tolerating up to 32 times the standard dosage of this antibiotic within just two months. The findings are published in PLOS Biology.
Treatment with vancomycin often disrupts the beneficial bacteria in the gut, leading to high rates of reinfection. As many as 30% of patients treated with vancomycin may experience another infection shortly after, with the likelihood of recurring infections increasing over time.
Despite the crucial role of vancomycin in UK healthcare, there is a lack of routine monitoring for resistance in clinical settings, which raises concerns that resistance may be developing unnoticed. If resistance becomes widespread, vancomycin could become ineffective as a treatment option in the UK.
Antimicrobial resistance (AMR) is recognized by the World Health Organization (WHO) as a significant global health threat. In 2019, AMR was directly linked to 1.27 million deaths worldwide and contributed to 4.95 million deaths overall.
Dr. Jessica Buddle, a Ph.D. student at the University of Sheffield and the study's lead author, stressed the importance of rigorous monitoring of vancomycin resistance in UK hospitals
The research team aims to explore the extent and mechanisms of resistance, model these conditions in the human gut, and work with UK epidemiologists to identify potential resistance patterns in hospital settings.
Although these resistant strains of C. diff evolve rapidly, they exhibit lower overall fitness, which might reduce their threat level. Additionally, these strains often have problems with sporulation, which is crucial for the bacterium’s transmission and survival on surfaces in hospitals.
Future research will focus on understanding how resistance affects the bacterium’s ability to cause severe disease and improving surveillance of emerging resistance in healthcare environments.

:max_bytes(150000):strip_icc():format(webp)/alec-baldwin-torino-film-festival-121824-3cf7cfbe5c4f4bcbb9197de4de062ea6.jpg?strip=all&resize=370,370)
:max_bytes(150000):strip_icc():format(webp)/Jimmy-Fallon-and-Prince-Harry-092624-baa1362d743d4f39a7d60bf57eb6e8b2.jpg?strip=all&resize=370,370)
:max_bytes(150000):strip_icc():format(webp)/randy-moss-121324-40b858c71b0f40bfa399e2fe00152b2a.jpg?strip=all&resize=370,370)
:max_bytes(150000):strip_icc():format(webp)/scandal-kerry-washington-121824-c51a2b5f0ef741268474bec2498c285a.jpg?strip=all&resize=370,370)
